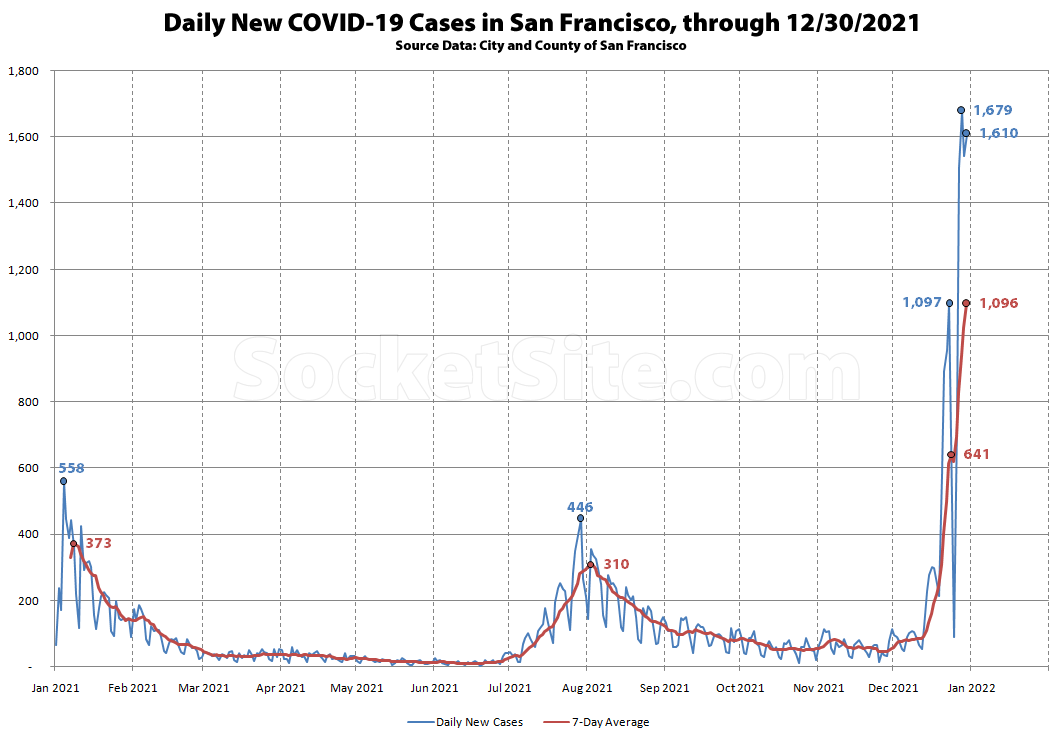
Based on our analysis of the City and County of San Francisco’s case data, the 7-day average number of daily new Covid-19 cases detected in San Francisco ticked over 1,000 on December 29 and was nearing 1,100 on December 30, despite the average being dragged down by a dramatic drop in testing on and around Christmas Day. And in fact, the 7-day average number of daily new Covid-19 cases detected in San Francisco is on pace to hit 1,500 within the next few days, with nearly 1,700 cases detected on December 28 and over 1,600 on December 30, counts which are likely to be upwardly adjusted.
At the same time and despite some local reports to the contrary, hospitalizations of people with Covid-19 in San Francisco have jumped, from 21 occupied beds at the end of November to 78 at the end of December, including 13 people in Intensive Care, with a typical lag of around 3 weeks between case rates and hospitalizations and a Delta peak of 123 hospital beds occupied by Covid-19 patients on August 15.
On a positive note, the Covid-19 test positivity rate in San Francisco might have peaked at around 18 percent in late December, with a local case rate of 192 new cases per 100,000 residents on December 28.
UPDATE (1/5): The number of new Covid-19 cases detected in San Francisco on December 30 has been upwardly adjusted to a record 1,753, for a 7-day average of 1,169 new cases per day, and climbing, while the number of people hospitalized with Covid-19 in San Francisco has jumped to 91, including 15 people in Intensive Care.
UPDATE (1/7): The number of new Covid-19 cases detected in San Francisco on December 30 has been upwardly adjusted to a record 1,812, for a 7-day average of 1,249 new cases per day, as of January 2, while the number of people hospitalized with Covid-19 in San Francisco has ticked up to 112, with 23 people in Intensive Care and an increase in occupancy rates (versus simply an increase in the mix of patients “with” Covid).
UPDATE (1/10): The number of new Covid-19 cases detected in San Francisco on December 30 January 3 hit a record 1,894, for a 7-day average of 1,297 new cases per day, while the number of people hospitalized with Covid-19 in San Francisco had ticked up to 135 as of January 5, with 25 people in Intensive Care and an increase in occupancy rates versus simply an increase in the mix of patients “with” Covid.
Expect the average daily new case count to drop over the next week or two with a post-holiday (party) reduction in testing, but the percent positive rate has yet to peak.
UPDATE (1/11): While the record number of new Covid-19 cases detected in San Francisco on January 3 has been upwardly adjusted to 2,464, a new record was set on January 4 with 2,616 new cases detected, for a 7-day average of 1,516 new cases per day, as originally projected above, and a test positivity rate of 20.7 percent.
At the same time, the number of people hospitalized with Covid-19 in San Francisco ticked up to 155 as of January 7, with 26 people in Intensive Care.
UPDATE (1/12): The record number of new Covid-19 cases detected in San Francisco on January 4 has been upwardly adjusted to 2,649, with a 7-day average of 1,589 new cases per day as of January 5 and a test positivity rate of 20.0 percent.
At the same time, the number of people hospitalized with Covid-19 in San Francisco has jumped to 177 as of January 8 and should total over 200 within the next couple of days, with 29 people in Intensive Care.
UPDATE (1/13): The record number of new Covid-19 cases detected in San Francisco on January 4 has been upwardly adjusted to 2,717, with a 7-day average of 1,662 new cases per day as of January 5 and a test positivity rate that’s still over 20 percent.
At the same time, the number of people hospitalized with Covid-19 in San Francisco ticked up to 186 as of January 9 with 33 people in Intensive Care.
UPDATE (1/14): The record number of new Covid-19 cases detected in San Francisco on January 4 has been upwardly adjusted to 2,777 with a 7-day average of over 1,600 new cases per day as of January 5 and a test positivity rate that’s ticked up over 21 percent.
And as projected above, the number of people hospitalized with Covid-19 in San Francisco ticked up to 203, as of January 10, with 36 people in Intensive Care.
UPDATE (1/19): While the number of new Covid-19 cases detected in San Francisco on January 4 has been upwardly adjusted to 2,832, the revised count for January 5 has been upwardly adjusted to a record 2,851.
On a positive note, the 7-day average number of new cases, which appears to have peaked at over 2,100 new cases per day on January 9, had dropped back down to a little over 1,500 per day as of January 13.
At the same time, the number of people hospitalized with Covid-19 in San Francisco had ticked up to 240, as of January 15, with 44 people in Intensive Care, numbers which are expected to continue to tick up over the next couple of weeks.
I’ll, again, be the broken record.
It’s never going away!
It’ll fluctuate up and down with variants, seasons, whatever, but the numbers will *never* be zero. Ever!
However, I won’t be surprised if at some point (when?) the tracking/reporting of the numbers will become something of interest to only hypochondriacs.
We’ve been there for many months already as far as my social circle is concerned. Hopefully SocketSite editor will join reality soon.
True! Covid is never going away. But that doesn’t mean we can’t be smart about how we deal with it.
Being concerned about Covid does not make one a hypochondriac. You would think that 800,000+ dead Americans would be recognition enough of this.
The vast majority of those 800k died of a virus that is meaningfully different from the one circulating now.
How do you define “meaningfully”? Omicron is a variant, but it’s still Covid.
This is just wrong. Even if you are talking about the major variants as “meaningfully different”, Delta is still wide spread.
CDC just said that Omicron is 95% of current cases detected.
I think we need to reach a level where we’re not losing 1000 people per day nationwide before this gets to the “seasonal issue” level.
Per the WHO dashboard, global COVID deaths for the last week ended Dec 27th was the lowest weekly level in 14 months. South Africa has seen no meaningful increase in deaths in recent weeks, despite Omicron originating there 2 months ago in the beginning of November. Omicron is highly contagious but much less dangerous than previous variants.
Closer to home, COVID deaths have started to tick up in San Francisco, with the sheer volume of cases starting to undermine the gains that have been made in vaccination rates, treatment options and the reduced severity of the Omicron variant, and despite the infancy of the local surge. And once again, there are significant negative impacts from a surge in cases beyond hospitalizations and/or deaths.
What are those negative impacts besides never ending fear of virus?
Shutdowns are a result of government actions not a virus.
As previously noted, there’s a growing list of workers, mangers and business owners who are suddenly dealing with unexpected “winter breaks” (in PR speak) from their normal wages, staffing levels and revenues, particularly in the hospitality, travel and retail sectors, along with a growing list of larger companies that are now pushing back their return to office dates (which has knock-on effects for both the residential and commercial real estate markets).
Lot of evidence about long term cognitive impairment, loss of smell, etc. accruing at this point.
I’m not a medical expert, but I’ve read opinions on long COVID that range from it being pure hypochondria to people who have an almost cult like belief in it. As a lay person, the following middle ground explanation someone told me seems to make the most sense.
If you get shot in the arm and are otherwise healthy you are very unlikely to die given the state of modern trauma medicine. They will take out the bullet and you will be “healed”. But that doesn’t mean that it won’t take a long time (or possibly never) for you to get 100% of your pre-injury functionality back. Nobody talks about “long bullet wounds”, it’s just a given that the medical priority is to treat the imminent danger to your life, but you make still have lingering problems from your injury.
In that context, it may not be that surprising that some people have longer term quality of life problems after a severe infection. Maybe “Long recovery from COVID” is a better term than “Long COVID”
“The crisis from the Omicron peak is not generated by serious COVID illness in regions with highly vaxxed populations,” Noble wrote in an email to SFGATE. “The crisis we are suffering in the Bay Area is largely driven by disruptive COVID policies that encourage asymptomatic testing and subsequent quarantines. … The vast majority of COVID-plus patients I take care of need no medical care and are quickly discharged home with reassurance.”
. . .
“Noble said that when she reviewed the charts on Jan. 4 at four UCSF campuses (UCSF Parnassus, Mission Bay, Mount Zion and Children’s Hospital of Oakland), she identified 44 hospitalized patients (both adults and children) with COVID. Of those, just 13 were admitted because of COVID. “I do not expect that number to increase substantially, or become unmanageable in the coming week,” she wrote. “The death rate in California is actually falling. And the predicted peak of cases is only about a week away.”
The remaining 31, or 70%, of patients tested positive after being admitted for unrelated reasons, including a hip fracture and a bowel obstruction. They’re all “completely asymptomatic or minimally symptomatic,” Noble said.”
As we’ve consistently noted and is currently playing out, both locally and elsewhere: “there are significant negative impacts from a surge in cases beyond hospitalizations and/or deaths.”
At the same time, while death rates are falling, absolute deaths are actually on the rise, “with the sheer volume of cases starting to undermine the gains that have been made in vaccination rates, treatment options and the reduced severity of the Omicron variant, and despite the infancy of the local surge,” as noted above.
Keep in mind that we’re only 39 days into the recent surge, which has yet to peak. At 39 days into the initial surge, back in the fourth quarter of 2020, there were only 74 people hospitalized with Covid in San Francisco. Discounting the 155 people that are currently hospitalized with Covid in San Francisco by 70 percent still yields 47 people hospitalized for Covid in San Francisco, which would be up from under 20, including all those “with Covid,” two months ago.
South Africa also did not have anywhere near this case rate. The nationwide U.S. case rate is currently at least 400% higher in every state than it ever was in South Africa. S.A. hit 40 per 100k and U.S. is currently at 300. Some U.S. states have recently set their all-time record-high death rates, including populous ones like Ohio. There are currently 1000s to 10,000s excess deaths every week in the U.S. so it’s no something to be blasé about.
If omicron turns out to not really kill people, that will be fine, but there is not yet any evidence to suggest that is the case. It’s too early to tell. The case rate doubled in the last two days, so it will be another 1-2 weeks before we know.
Note to Editor….are you that hellbent on censoring descending opinion? Or afraid of descending opinion?
While we prefer to address incorrect statistical claims and conclusions directly, in the light of day, we draw a line at clinical misinformation (which doesn’t represent a censoring of “dissenting opinions” but rather an intolerance for dangerous “alternative facts”).
“The concept of “incidental COVID” — where patients who are in the hospital for other reasons other than COVID-19 are found to be COVID-19-positive and subsequently counted in coronavirus hospitalization numbers — has always existed, but is being discussed more widely as the omicron variant causes more asymptomatic cases than previous strains. UCSF’s Dr. Bob Wachter said that incidental COVID leading to inflated totals was a “non-issue” in the past but a “bigger issue” now, while top national advisor Dr. Anthony Fauci raised the “with COVID” vs. “for COVID” distinction…”
Being hospitalized “with COVID” isn’t really a great situation to be in either.
People point out that the seriously bad COVID outcomes are much less common in the otherwise healthy. But the flip side of this is that COVID is a much more serious threat to people who are not otherwise healthy. And people who are in the hospital for other reasons are very likely not to be otherwise healthy.
With each passing spike, people will care less and less. My guess is that this is the last one that meaningfully changes behavior (cancelling a vacation / event, mask rules returning, etc). Hopefully the analysts are correct and the pandemic should be effectively over by early February, with return to office by March/April.
Spoken like one who puts padding petty cash over saving lives. When will we stop trying to thread the needle and take real steps to get on top of this thing?
What would you recommend we do to “get on top of” COVID at this point? Not sure if you’re referring to domestic, SF, international or something in between, but vaccines, lockdowns, masks and social distancing have worked to some extent, but not enough. What other tools do we have in our toolshed?
#1 Shut down indoor events. I love going to Warriors games, but they should be played without fans. Same with live music, nightclubs.
#2 Require that no one flies without proof of vaccination or negative test.
Though we should have done these a long time ago.
Does anyone have data on excess deaths? With so many covid cases, it seems likely to me that some number of them are people who would have died anyway but happened to get covid just before they died. Similar for hospitilizations, I’m curious how many people would have been in the hospital anyway due to some other cause and since there is so much covid around now they tested positive.
National Center for Health Statistics: Excess Deaths Associated with COVID-19
Don’t know if this is done at the local level (would be kind of hard since people move around a lot w/i states)
IHME provides a state level estimated “excess death” count. For clarity to people who don’t know the excess death concept they call it the “Total” number, and you need to click on that option to show it.
In their model, the number of people who “would have died anyway” is much smaller than the number of deaths that have occurred that are unattributed to covid19, but statistically exceed what was expected by historical trends.
Reported Covid deaths in California are about 75k, and IHME calculates an excess death range of 75k to 135k, with their likely scenario at 93k.
It is a modeled and analytic result, so pick how much you want to trust it, but they do document their process and provide their parameters.
It seems like you have a view not based on data and are trying to find anything to backsolve into your feeling. The notion of people being in the hospital not for covid is valid now with omicron but not material with prior variants. There are indeed people in the hospital with covid who might have died on a similar timeframe. And there are many people who have died globally without being counted as covid deaths. Fwiw, in previous disease outbreaks, excess mortality is frequently revised higher in studies years later.
UPDATE: The number of new Covid-19 cases detected in San Francisco on December 30 has been upwardly adjusted to a record 1,753, for a 7-day average of 1,169 new cases per day, and climbing, while the number of people hospitalized with Covid-19 in San Francisco has jumped to 91, including 15 people in Intensive Care. Hospitalizations typical lag case rate by 3 weeks and at the peak of the Delta surge there were 123 hospital beds occupied by Covid-19 patients in San Francisco.
The rate of Covid-19 hospitalizations among children (0-17) in the US DOUBLED OVER THE PAST WEEK to an all-time high, admission rate is twice as high as it was for Delta.
Right, but the question is a matter of “with” covid or “for covid,” all capitalizations notwithstanding.
I think the distinction will turn out to be a red herring. Quotes from the Guardian:
“We have about four times as many children admitted currently as we have had in any other wave,” Dr Elaine Cox, the chief medical officer for Riley Children’s Health in Indiana, told reporters on Tuesday. They are also seeing the severity rise among the children who are admitted to the hospital, Cox said. “So there are more of them, and they are sicker.” More than half the hospitalized children have had to spend time in the intensive care unit, and at least 40% of those kids need to be put on a ventilator…”
“In New York, hospitalizations among kids quadrupled. In Washington DC, children’s hospital admissions have roughly doubled. In Texas, children’s hospitalizations were described as “staggering”. In Alabama, cases were “like a rocket ship”. In Louisiana, one doctor said: “We’ve never seen anything like it.” In Ohio, one associate professor of internal medicine and pediatrics critical care recently told ABC news: “We’re on fire.”
I don’t. I think the overriding 4X numbers for u-18 is precisely on par with what South Africa saw. I think the severity remains low, and I think that relatively speaking, using percentages for a 354 bed hospital in Indianapolis is rather misleading. Think in terms of what that looks like at that Indiana hospital. Say, 20 kids, 10 spend “some” time in the ICU, 4 on a ventilator.
I don’t mean to be callous and I’m just as worried about this as the next parent, believe me. However we seem to keep on conflating percentages and figures across metrics when we speak about this virus and its mutations.
You are wrong on all counts, stop spreading misinformation to try to game a personal wish outcome! Severity is not low if you are hospitalized. South Africa is one data point from a country not known for health care system or records. Stop hypothesizing numbers fitting the 4x scenario, that is just lazy.
Frankly, you don’t sound worried at all and you certainly don’t have young kids.
Yes I do, yes I am, you’re wrong, I’m not spreading misinformation, the 4X mark in the citation of the person I was speaking to coincides with the SA rate. Your citation is a much smaller mark still when it comes to pediatric rates. I’m not sure why such a non-take as yours was allowed to stand, frankly. Go rave ad hominems at someone else I’m not here for talking to someone I’ve never engaged with who was rude for no reason.
Head of COVID response for UCSF’s ER dept.: ‘I have not intubated a single COVID patient during this Omicron surge’
After reviewing the charts of every COVID-positive patient at UCSF hospitals on Jan. 4, Dr. Jeanne Noble, an associate professor of emergency medicine at UCSF, determined that 70% of them were in the hospital for other reasons.
Last week, the U.S.’s top health official Dr. Anthony Fauci said that “it is much more relevant to focus on the hospitalizations as opposed to the total number of cases.”
So if it is relevant to focus on the number of hospitalizations, surely you would agree that the number of hospitalizations in San Francisco is way up, right?
The numbers of hospitalized could be over stated by as much as 70% per Dr. Jeanne Noble, associate professor of emergency medicine at UCSF.
As previously outlined, we’re now 40 days into the recent surge, which has yet to peak.
At 40 days into the initial surge, back in the fourth quarter of 2020, there were only 81 people hospitalized with Covid in San Francisco. Discounting the 175 people that were hospitalized with Covid in San Francisco as of January 8 by 70 percent still yields 53 people hospitalized “due to Covid,” which would be up from a discounted “6” at the start of the surge.
From where does the language “due to covid” attribute? Secondly any statistics regarding how many of them are treated and immediately released?
It’s based on the hypothesis that 70 percent of the current Covid-19 hospitalizations in San Francisco are patients that are hospitalized “with” Covid and only 30 percent of the hospitalizations are “for” / “due to” Covid.
We don’t have any statistics on the average length of stay or acuity levels, but keep in mind that the hospitalization stats we quote represent the net number of beds occupied, not admissions (i.e., an immediate discharge wouldn’t increase the count); Intensive Care counts are ticking up; and Covid deaths have started to tick up as well.
Matt Allenford, what happened to your argument that hospitalizations were low and not increasing?
If the jump in Covid hospitalizations is actually being driven by “with” versus “for” Covid cases, we shouldn’t see a jump in hospital admission or occupancy rates over the next few weeks, which would be great news.
Anthony Fauci: “If you look at the children are hospitalized many of them are hospitalized with COVID as opposed to because of COVID,” Fauci said when addressing reports of increased pediatric hospitalization. “What we mean by that is that if a child goes in the hospital they automatically get tested for COVID and they get counted as a COVID hospitalized individual, when in fact they may go in for a broken leg or appendicitis or something like that. So it’s over-counting the number of children who are ‘hospitalized’ with COVID as opposed to because of COVID.”
UPDATE: The number of new Covid-19 cases detected in San Francisco on December 30 has been upwardly adjusted to a record 1,792 while the number of people hospitalized with Covid-19 in San Francisco has ticked up to 97, as of January 2, including 19 people in Intensive Care, which is up from 5 in late November and having doubled over the past week.
On October 2, there were 26 people in Intensive Care, which is 7 less than we have now.
The question is… why do you choose a narrative of fear? I’m trying to rent apartments, buy buildings conduct business in real estate. A narrative of fear is not good for the mental health of the city. We need to get on with our lives. If there were 10,000 positive cases and 1,000 in the hospital, we still need to move humanity forward without fear. Everyday there are risks, we live with risks, we move forward in the face of risks.
A couple of weeks ago you proclaimed that hospitalizations were low and remained flat. That is obviously no longer true. Why do you choose a narrative of ignorance?
Like you, I wish that Covid had never happened. I also wish that my family and friends, including those who are immunocompromised or unable to be vaccinated, stay alive.
A couple weeks ago that was true. Was it not? I look at omicron and I see a variant that is clearly much more infectious than previous variants, yet hospitalizations to date are not even at delta levels. Is that nothing? Do you not rate those developments? and, “stay alive” ? Omicron is not killing people by and large. So yes by all means stay alive. Be careful. Follow safe practices. But this variant is what it is, singularly. So why can we not tailor our language to discuss this variant now?
Yes, but it is completely ignorant to mention that hospitalizations remain flat at the start of a wave of infections. Of course they are flat at that time. The point is that they will rise.
As for “staying alive”, plenty of people are hospitalized due to illnesses unrelated to Covid. Hospitals are now having trouble finding beds because so many beds are being taken up by people infected with Covid. I have direct first hand experience with this. Hospital staff are shuffling people around individually so as to find beds for everyone. So yes, “staying alive” is no exaggeration.
Which is not to minimize the actual health risk from Omicron itself. Yes, is seems to be less dangerous than other variants, though of course the long term effects are not known, but my colleagues and friends who are doctors on the front lines of treating patients will assure you that it is still dangerous.
I have friends in the trenches on numerous fronts too and yes they echo the things your circle says. I also have extended family who have it right now, and these same people caught earlier variants to scary effect. The differences wrt symptoms are stark. None of this is say that it won’t ravage the unvaccinated or the immunocompromised. (Which, by the way, some of my people are.) But I won’t sit there and let folks jump willy nilly among metrics past and present and allow someone to harangue me about percentages from an article, which when you dig in, is merely a singular hospital’s percentages, etc. This is a greatly contagious variant with much milder, briefer symptoms. Therefore hospitalizations will likely be high but shorter. How that dynamic effects systems is playing out in real time. I don’t have the wherewithal to compare hospital stay lengths, higher admittance but quicker cycling of beds vs harsher symptoms and longer stays. I doubt that data even exists yet anyway though it’ll probably be the next significant set to examine.
Judging the severity of a new strain, based on the relative experiences of people who caught an earlier strain, developed antibodies, recovered and were then re-infected, would be a mistake. Regardless, ICU occupancy rates are ticking up, not simply hospitalizations. And deaths from Covid have started ticking up as well, despite the infancy of the latest surge.
Indeed. Anecdotally I could just as easily have pointed to people I personally know who never caught it up till now and are only experienced mild symptoms, people who had the initial variant, delta, non-vax’d, vax’d, etc etc. Anyway, it’s not as if I didn’t qualify my anecdotes with language speaking to significant risk remaining. It’s generally pretty easy to pick apart language at any given time when it comes to coronavirus takes. What, is everyone supposed to write a study-link-laden discertation each and every utterance? Come on. You qualifying everything is also noise.
We were simply responding to the only anecdotes you offered (“I also have extended family who have it right now, and these same people caught earlier variants to scary effect. The differences wrt symptoms are stark.”).
The fact that we have a highly vaccinated population, along with a fair number of people who have recovered from a prior infection, is one of the reasons the current strain is presenting as less severe. At the same time, the spike in hospitalizations amongst children, which is dramatically different from earlier in the pandemic, is the relatively low vaccination rate for those under 12 years of age and particularly for those under the age of 5.
And once again, ICU occupancy rates are ticking up in San Francisco, not simply hospitalizations. And deaths from Covid have started ticking up as well, despite the infancy of the latest surge.
Anyway, again, kids didn’t go the hospital that much in South Africa during its pre-Omicron variant outbreaks either. Low vax rate country. High previous infection rate country. Low omicron death rate. To the person who is next going to say, as I saw previously, “yes but SA does not supply reliable data” first off, that’s pretty racist if you think about it. Secondly, Denmark certainly looks similar.
Unfortunately, there were more Covid deaths in the U.S. on January 4 than on any one day during the Delta surge, in fact the most deaths in a day since February of last year. And the average number of daily Covid deaths in the U.S. is ticking up, locally as well.
Indeed, how so? I look at that chart and see delta deaths are much higher than omicron.
That’s correct, hospitalizations and Intensive Care occupancy rates were trending down from October to November and into December, a trend which has since reversed and shouldn’t catch any plugged-in readers by surprise.
And as always, we choose a narrative of knowledge and data-driven decision making, not ignorance or “fear.”
UPDATE: The number of new Covid-19 cases detected in San Francisco on December 30 has been upwardly adjusted to a record 1,812, for a 7-day average of 1,249 new cases per day, as of January 2, while the number of people hospitalized with Covid-19 in San Francisco has ticked up to 112, with 23 people in Intensive Care and an increase in occupancy rates (versus simply an increase in the mix of patients “with” Covid).
In addition, based on preliminary data from the State, the number of people hospitalized in San Francisco with Covid surpassed the Delta peak yesterday, January 6.
At the peak of the Delta surge there were 95 available ICU beds in San Francisco. And based on data from the State, yesterday there were 76 available ICU beds in San Francisco.
UPDATE: The number of new Covid-19 cases detected in San Francisco on
December 30January 3 hit a record 1,894, for a 7-day average of 1,297 new cases per day, while the number of people hospitalized with Covid-19 in San Francisco had ticked up to 135 as of January 5, with 25 people in Intensive Care and an increase in occupancy rates versus simply an increase in the mix of patients “with” Covid.Expect the average daily new case count to drop over the next week or two with a post-holiday (party) reduction in testing, but the percent positive rate has yet to peak.
UPDATE: While the record number of new Covid-19 cases detected in San Francisco on January 3 has been upwardly adjusted to 2,464, a new record was set on January 4 with 2,616 new cases detected, for a 7-day average of 1,516 new cases per day, as originally projected above, and a test positivity rate of 20.7 percent.
At the same time, the number of people hospitalized with Covid-19 in San Francisco ticked up to 155 as of January 7, with 26 people in Intensive Care.
UPDATE: The record number of new Covid-19 cases detected in San Francisco on January 4 has been upwardly adjusted to 2,649, with a 7-day average of 1,589 new cases per day as of January 5 and a test positivity rate of 20.0 percent.
At the same time, the number of people hospitalized with Covid-19 in San Francisco has jumped to 175 as of January 8 and should total over 200 within the next couple of days, with 29 people in Intensive Care.
UPDATE: The record number of new Covid-19 cases detected in San Francisco on January 4 has been upwardly adjusted to 2,717, with a 7-day average of 1,662 new cases per day as of January 5 and a test positivity rate that’s still over 20 percent.
At the same time, the number of people hospitalized with Covid-19 in San Francisco ticked up to 186 as of January 9 with 33 people in Intensive Care.
UPDATE: The record number of new Covid-19 cases detected in San Francisco on January 4 has been upwardly adjusted to 2,777 with a 7-day average of over 1,600 new cases per day as of January 5 and a test positivity rate that’s ticked up over 21 percent.
And as projected above, the number of people hospitalized with Covid-19 in San Francisco ticked up to 203, as of January 10, with 36 people in Intensive Care.
UPDATE: While the number of new Covid-19 cases detected in San Francisco on January 4 has been upwardly adjusted to 2,832, the revised count for January 5 has been upwardly adjusted to a record 2,851.
On a positive note, the 7-day average number of new cases, which appears to have peaked at over 2,100 new cases per day on January 9, had dropped back down to a little over 1,500 per day as of January 13.
At the same time, the number of people hospitalized with Covid-19 in San Francisco had ticked up to 240, as of January 15, with 44 people in Intensive Care, numbers which are expected to continue to tick up over the next couple of weeks.